When my egg shattered (aka: when I accepted myself as trans) I found myself with pretty much no dysphoria surrounding my phallus. This was, in fact, one of many reasons I had convinced myself I wasn’t trans for so long, I didn’t hate my junk (this changed, but I’ll get to that later). What I did know almost immediately, however, was that I needed to lose the testosterone factories. I hated my testicles with a mad passion, they had provided me with nothing but literal pain for my entire life (also my children, but that is not a saving grace). For, you see, I had a medical condition which had never been discovered and never was treated; a testicular torsion so severe that it pulled the entire testicle up into the inguinal canal, where it could be gradually crushed by my pelvic joints.
This is the problem when you’re an obese teenager; when you tell someone that your groin hurts too much to keep running in gym class, they just immediately write you off as lazy and making up excuses to get out of doing what everyone else does. Fatphobia was and still is extremely rampant, and no one, not doctors or my mother, ever bothered to look beyond that layer of child blubber that gender dysphoria had pushed on to me. So for the entirety of my teen years, this problem was undiagnosed and thus untreated. By the time I was 20 years old, that little T factory was a pile of rubble, but that didn’t stop it from hurting. I have had chronic testicular pain for my entire life.
Thus, when I found out that a gender transition gave me a reason to get rid of those pain orbs, I was SO on board. It ultimately took over a year for it to happen, and this is that story.
Getting the balls rolling
It started with an orchiectomy consult on February 5th, 2018, with Dr T. Mike Hsieh (pronounced Shay), the Associate Professor of Urology at UCSD Health. I found out about Hsieh from a friend who I knew was exceptionally methodical in her research and was very pleased with her initial consult with him. Our consult was very straight forward; he was very nice, personable, listened to all my concerns and answered my questions, and most importantly completely understood transition needs. He explained that his bilateral incision method would post no issues for future vaginoplasty. I explained to him about my chronic pain issues and tried to stress that this was my primary reason for wanting the surgery, and it seemed like he understood.
I was put in touch with his executive assistant so I could schedule the surgery, and went on my way. When she got back to me I was astonished to find out she was scheduling me for just three weeks later on February 26th. That never happened tho, because Blue Shield (my insurance) did not come through in time with approval. Hsieh had submitted the claim with a gender transition related code, which made approval significantly more complicated, as having a GID (Gender Identity Disorder) code makes it into a gender confirmation surgery, activating all kinds of special requirements. If Hsieh’s office had submitted it as treatment for chronic pain, I wouldn’t have even needed pre-auth. The next week I was informed that Blue Shield required multiple letters from therapists showing that this procedure was “medically necessary” for me to get it. I scrambled to get a letter from my therapist, as well as a doctoral psychologist. February 26 came and went, and I was rescheduled for March 12th.
On March 5th I found out I had been rejected by Blue Shield. In order to secure pre-auth, I had to have a letter from my prescribing physician stating that I had been on hormone therapy for over a year. It had only been 10 months. They could not even begin to process a new authorization attempt until one year had come and gone. This is based on a WPATH recommendation of one year spent on hormones to ensure the patient really is certain that they are transgender; it’s a guideline, not a rule, and my therapist was furious they were treating it as such. My surgeons assistant told me to call back the first week of May.
Fast forward two months later, I contact again, and find out that the soonest they could book me for another surgery was June 25th; Hsieh was fully booked for a month and a half. In the mean time they started the pre-auth process again. A week went by with no news, then two weeks. I called to find out if there was any updates, they called Blue Shield, and Blue Shield claimed they had never received a pre-auth (PA) request. So they sent it in again, and again two more weeks went by with no response. This time BS said they had to schedule a peer-to-peer conversation with the surgeon, because the first PA had been rejected, but nobody at Blue Shield seemed to agree on how that should happen. I started getting ancy, because I had a trip booked for the week prior to my surgery and I did NOT want to be trying to get this approved while in a hotel room in Denver.
On June 15th I received a phone call from a liaison at Blue Shield. She was personally calling to inform me that she had approved my surgery. I thanked her profusely.
Making the cut
The Monday before the surgery I received a call from an anesthesiologist at UCSD Medical to go over all the necessary pre-op instructions.
- I was to stop taking any vitamins or supplements 3 days before the surgery, as well as my ADHD meds. I asked if there were any issues with my HRT and she said it was all fine, tho I could stop taking the Spironolactone if I wished (I did).
- I needed to go out and buy a surgical scrub soap and use it on my entire body three times before my surgery (twice the day before, and again that morning)
- Absolutely no food or drink after 8pm the night before or the morning of (this became clear why after I woke up from surgery).
- I could not drive myself to the hospital, and I needed a loved one to bring me home. No Ubers.
One amusing part of the conversation was when she asked me how physically active I was, and I responded “Lethargic”. “Why is that?” “Because I’m lazy.” She laughed and recited as she wrote down: “Can exercise, chooses not to.” She also didn’t know that spiro is taken as an anti-androgen and found that very interesting. My check-in time was 9:00, surgery would start at 11, I should be in recovery by noon and expected to be released at 2pm.
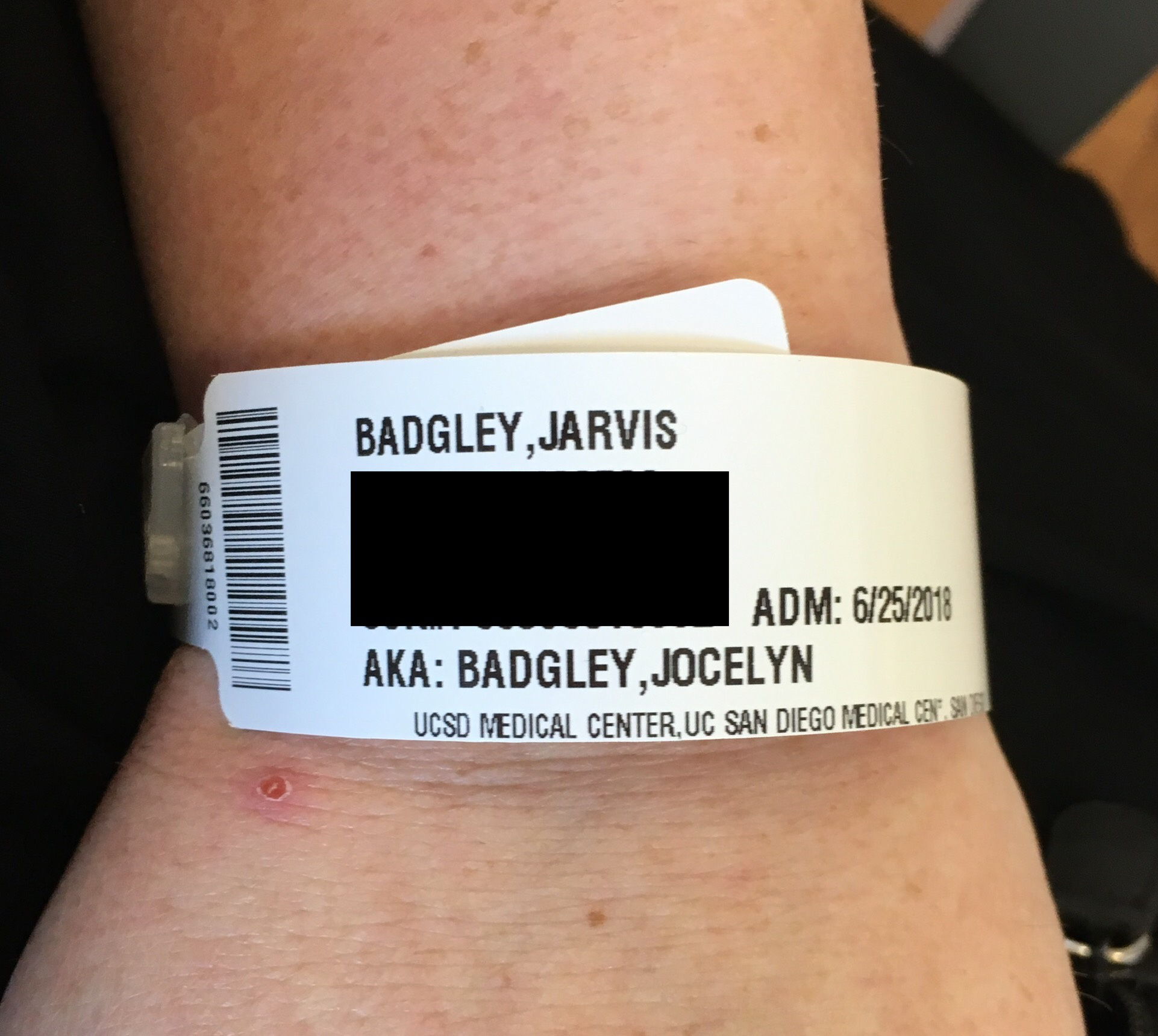 At this point Jocelyn had already been my legal name for two months, but UCSD still had me on file as Jarvis because I had first seen the surgeon before my name change.Due to schedule conflicts with getting my daughter to school and my son babysat, my wife was not able to drive me to the hospital, but a friend was willing to oblige me on his way to work. I arrived a little before 9 and went straight to admitting. My co-pay for the hospital stay was $520, which I expected, and had to pay in advance. I had started the entire process before my name change happened, and despite informing multiple people of the legal change, they never got their system updated. Thus, when I was given my wrist band, I was frustrated to discover that it still had my deadname on it. It did, however, list Jocelyn as my preferred name. I then went up stairs to check in for outpatient surgery.
At this point Jocelyn had already been my legal name for two months, but UCSD still had me on file as Jarvis because I had first seen the surgeon before my name change.Due to schedule conflicts with getting my daughter to school and my son babysat, my wife was not able to drive me to the hospital, but a friend was willing to oblige me on his way to work. I arrived a little before 9 and went straight to admitting. My co-pay for the hospital stay was $520, which I expected, and had to pay in advance. I had started the entire process before my name change happened, and despite informing multiple people of the legal change, they never got their system updated. Thus, when I was given my wrist band, I was frustrated to discover that it still had my deadname on it. It did, however, list Jocelyn as my preferred name. I then went up stairs to check in for outpatient surgery.
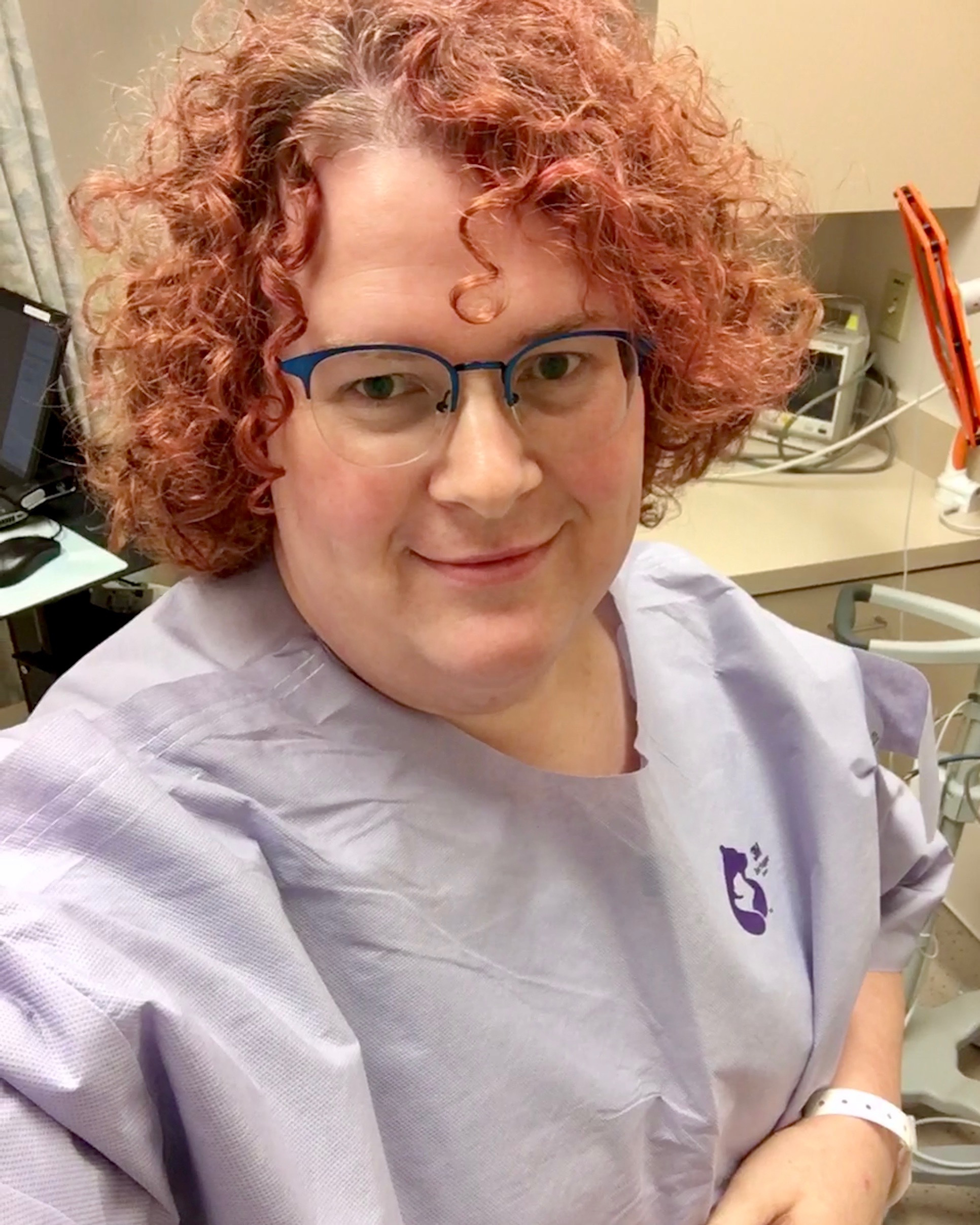 A nurse took me back to a prep room where I was given a surprisingly technical paper robe to change into (there were neat little flaps all over it for monitoring equipment, and I needed her help getting in to it). She took my vitals and then set to work on getting me an IV, and it was indeed work. I do not have very visible veins, phlebotomists struggle with my arms every time I get blood drawn. Thankfully, I knew a trick from one such phlebotomist, get the arm really hot. It makes the veins pop out and become extremely clear. Unfortunately, that still didn’t make it possible for her to get one in my forearm, so she had to do my hand.
A nurse took me back to a prep room where I was given a surprisingly technical paper robe to change into (there were neat little flaps all over it for monitoring equipment, and I needed her help getting in to it). She took my vitals and then set to work on getting me an IV, and it was indeed work. I do not have very visible veins, phlebotomists struggle with my arms every time I get blood drawn. Thankfully, I knew a trick from one such phlebotomist, get the arm really hot. It makes the veins pop out and become extremely clear. Unfortunately, that still didn’t make it possible for her to get one in my forearm, so she had to do my hand.
I haven’t had an IV done in a long, LONG time, not since I was hospitalized for pneumonia at the age of seven. That particular incident was especially traumatizing, first because the admitting nurse tried to put an adult catheter into the veins of a seven year old, causing me severe pain. The other reason is because I started sleep walking while I was there and pulled the IV out of my arm at least three times. 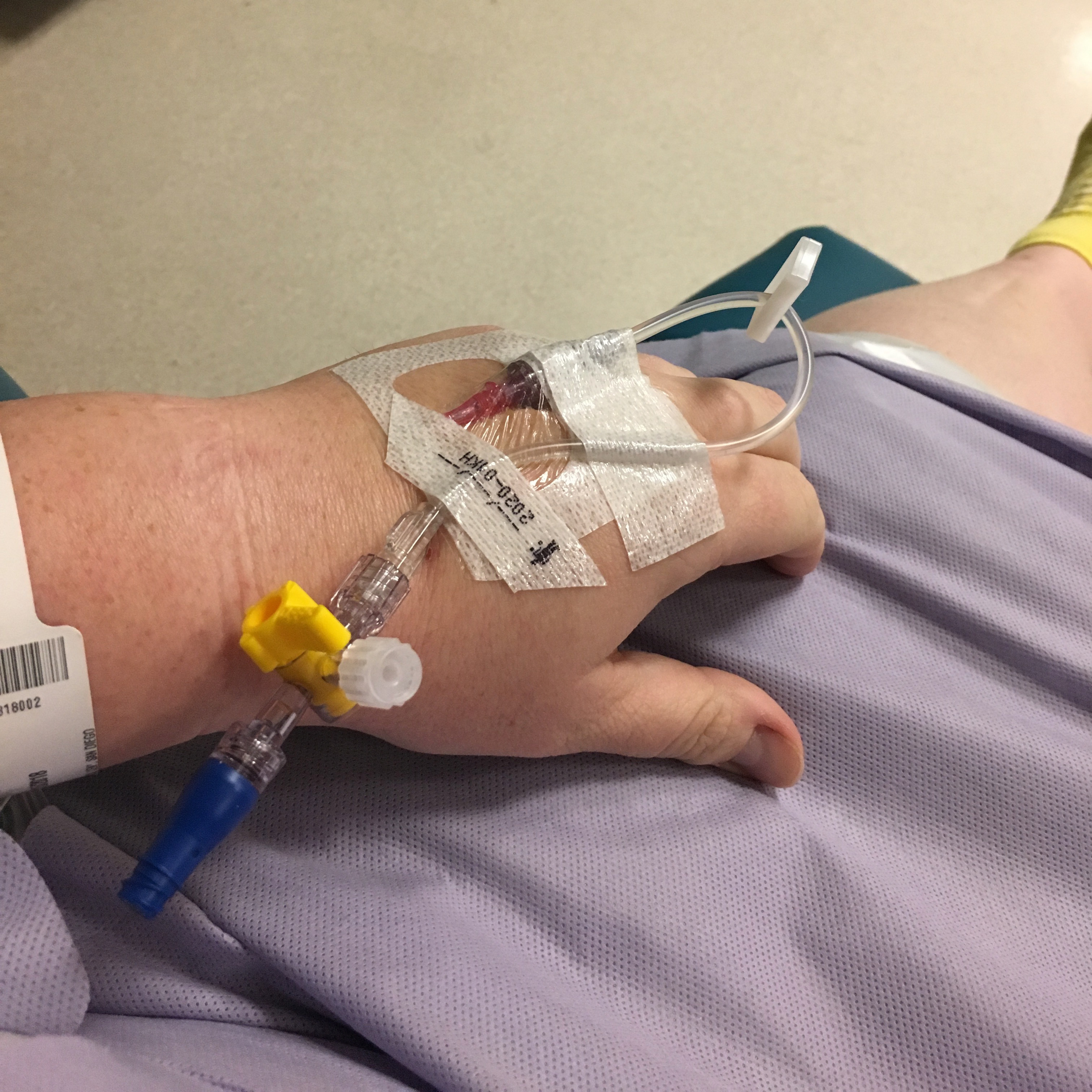 Now, the antiseptic they use for an IV has a very unique smell, and that smell caused all that childhood trauma to come rushing back. My anxiety went through the roof, and the entire experience left me desperately trying to control a panic attack. The nurse clearly could tell what was happening and was doing her best to calm me through it, but it sucked. She managed to get it on the first stick tho, got me taped up well, and after 5-10 minutes I was back to calm. They then moved me down the hall to pre-op observation. I then sat in a bed for about an hour and a half.
Now, the antiseptic they use for an IV has a very unique smell, and that smell caused all that childhood trauma to come rushing back. My anxiety went through the roof, and the entire experience left me desperately trying to control a panic attack. The nurse clearly could tell what was happening and was doing her best to calm me through it, but it sucked. She managed to get it on the first stick tho, got me taped up well, and after 5-10 minutes I was back to calm. They then moved me down the hall to pre-op observation. I then sat in a bed for about an hour and a half.
My wife wasn’t able to leave our house until 10am, so the entire time I was stressing about if she would arrive on time to see her before they took me into the OR. I’d been persistently checking Find My Friends to watch how she was coming. My surgeon arrived around 10:45am to see how I was doing and to tell me my post-care instructions. He asked if my wife was coming (he’d met her at the consult), and I held up my phone and said “Yes, she’s just a few blocks away!” He laughed and said “Well I’ll have to tell her all this as well, because you’re not going to remember this conversation.”
Let me tell you, “you’re not going to remember this conversation” is are the weirdest thing to have someone say to you (especially since I do remember it). I sat there just laughing at the entire concept.  He left to go prep for surgery, and then my wife Katharine arrived. I did not realize just how much anxiety I was having until she walked into the room and I suddenly felt a whole lot better. Having her there at my bedside was a massive relief.
He left to go prep for surgery, and then my wife Katharine arrived. I did not realize just how much anxiety I was having until she walked into the room and I suddenly felt a whole lot better. Having her there at my bedside was a massive relief.
The anesthesiologist and his student arrived shortly after and went through all the usual questions (the same questions I was asked probable ten times that day). He informed me that when it was time to go in they would come hook up a sedative to the IV to calm me as I was being transported, and then they would start the actual anesthetic once I was on the OR table. They didn’t actually end up doing that for almost another 30 minutes, so surgery started a little late.
I remember them starting me on the IV, Katharine taking my things, and my bed being wheeled out of the room. At the time I didn’t feel like the sedative was doing anything, but now that I look back on it I can see how much calmer I suddenly was as we were moving. We had small talk about living in San Diego while we walked the corridors, as the OR was on the other side of the building. They wheeled the bed against the OR table and I slid over. Numerous instrumentation was attached to me, and my arms were strapped down. The last thing I remember was an oxygen mask being fitted over my face, and not quite fitting correctly, so the orderly was wrestling with it. I don’t remember falling asleep, my memory just stops.
Then I woke up in post-op observation, blearily looking around enough to realize where I was. A nurse was working at the station next to me, but didn’t seem to have noticed I was awake. Then I threw up. I tried to tell her I was going to, I could feel it coming, but my body wasn’t responding enough to get the warning out. She quickly reacted, shoving a cup into my hands and putting it against my mouth. I think I threw up three times. I remember her telling me that it was normal to be nauseous from the anesthetic (this is why I was fasting) and that they were going to give me some IV anti-nausea medication to counter it, but it would put me back to sleep. I think I passed back out before they did it. Katharine wasn’t there, but I expected that. She had to go pick up our daughter from school and then come back.
 Kat was at my side when I came to. I was extremely groggy and barely able to communicate. I asked what time it was, but she said “You wouldn’t understand it if I told you, but you’ve been out for a few hours”. The nurse informed me that she was there covering for the other nurse I’d had earlier, who was on break. I know I drifted in and out of consciousness for a while. The temp nurse misgendered me once, my wife immediately corrected her, and didn’t need to after that. It was the one and only time I was mis-gendered while at the hospital. The UCSD staff were always very conscious of my gender, and on one occasion a nurse explicitly asked me what pronouns to use.
Kat was at my side when I came to. I was extremely groggy and barely able to communicate. I asked what time it was, but she said “You wouldn’t understand it if I told you, but you’ve been out for a few hours”. The nurse informed me that she was there covering for the other nurse I’d had earlier, who was on break. I know I drifted in and out of consciousness for a while. The temp nurse misgendered me once, my wife immediately corrected her, and didn’t need to after that. It was the one and only time I was mis-gendered while at the hospital. The UCSD staff were always very conscious of my gender, and on one occasion a nurse explicitly asked me what pronouns to use.
I started shaking, hard, as hard as the worst fever I’ve ever had. I didn’t exactly feel cold, but the nurses wrapped me up in a blanket and put a heating tube under it, and that calmed down the shivering after a bit. I later found out that this is extremely common when coming up from general anesthesia. The brain thinks the body is dying, so it starts trying to jolt it awake. That lasted for probably 2-5 minutes (time tracking is hard when you’re that doped up).
I must have passed out again, because when I woke up a different nurse was there. “Hi, do you remember me?” I shook my head. It turned out she was the one who gave me the cup when I woke up the first time. Gradually over the next half hour I got more and more aware and able to move my body again. At some point I realized I wasn’t wearing the gown I’d been in when I entered the OR. Changing that could not have been easy, I am not a light woman.
Eventually I was alive enough that they decided I was ready to go home. Kat went out to bring the car up while I got dressed. Getting my shirt on was fairly easy, but then getting off the bed to put on my skirt took some time. After I was dressed they sat me down in a wheelchair and took me out to the street. I realized as we were going that I didn’t know who was pushing my wheelchair, but I lacked the wherewithal to turn around and see. When we got into the elevator a man’s hand reached out to push the button, and I thought “Oh.”
Getting out of the wheelchair and into the car was easier than I expected, but still a trial. I got belted in, Kat got into the drivers seat, and we started to pull away. Immediately I got hit with motion sickness and threw my arm behind me to grab anything I could puke into. There happened to be an empty starbucks cup, and I can remember dry heaving into it a few times before things settled down. I remember getting very angry as we left the hospital, because it seemed like the GPS was telling Kat the wrong way and she ended up going in circles around the hospital.
The roads in that part of town (well, in most of San Diego City) aren’t well maintained, and the car kept lurching a lot, making it harder and harder to not throw up. I find the experience funny now, but Kat doesn’t remember the experience fondly. She says it was my fault she made the wrong turn, and I was being an asshole about it. I fell asleep before we got on the freeway, and didn’t wake up until we got home. Kat led me into the bedroom where I collapsed into bed and stayed there for the next few hours. It was 4:30pm, according to the timestamp on this photo. I fell asleep shortly after.
An Empty Sack
 I woke up around 6:00 as Kat was getting the kids to bed. My hunger was fierce, as I had not eaten anything in 24 hours, and my body was desperate for nutrients. However, Kat was also worried about me eating anything too strong because I was still coming down off the anesthesia and could be nauseous. I don’t remember exactly what I ate, I think there were a lot of chips, but whatever it was didn’t satiate my hunger.
I woke up around 6:00 as Kat was getting the kids to bed. My hunger was fierce, as I had not eaten anything in 24 hours, and my body was desperate for nutrients. However, Kat was also worried about me eating anything too strong because I was still coming down off the anesthesia and could be nauseous. I don’t remember exactly what I ate, I think there were a lot of chips, but whatever it was didn’t satiate my hunger.
Going to the bathroom was a challenge. I had left the hospital with the typical hospital issue disposable underwear, but crammed full of a giant wad of cotton gauze. It was like walking around with a diaper on. I kept that on for the first day, so when I went to the bathroom for the first time I had to pull that down and keep it together when I pulled it back up. For the first 36 hours after the surgery I couldn’t actually tell when I needed to pee, everything down there was in a state of shock, and all the wires were crossed.
Pain was surprisingly low. It was definitely present, but after a life of chronic testicle pain, this didn’t seem all that worse. I felt no pain at all from the incision. The suture was small, about one inch long, starting at the base of my penis and down along the perineal raphe. A surgical glue was laid over top of the stitches, and a bandage over that. There was no blood at all, and the entire area was very clean. I also realized that my entire groin had been completely shaved. The pain I felt was much deeper, and the swelling was real.
 𝓙𝓸𝓬𝓮𝓵𝔂𝓷
𝓙𝓸𝓬𝓮𝓵𝔂𝓷 
 ⚢
⚢ @TwippingVanilla
@TwippingVanilla It’s 4:30am, 13 hours since I left the hospital, and I just found another probe that the nurses forgot to remove from my body. (This makes two).
The tips of the spermatic cord swell up from blood pooling at the tips, forming balls almost as large as the testicles themselves. The inguinal canals also swell up, making things very puffy. Walking around was a slow processes for the first two days, just because everything was so sensitive and enlarged. My penis itself had completely contracted, to the point it was a solid centimeter below the surface. This made peeing difficult, as the urine just pooled in the cavity. Kat made the joke that it was in hiding after that nice couple across the street had been murdered in a brutal home invasion. This lasted for the rest of the week.
My aftercare instructions were that I could take a shower the next day, but not to wash the incision directly. It was ok if it got wet, but I shouldn’t directly spray it. They also told me I shouldn’t immerse the wound in water, so now baths or swimming for 6 weeks. I ended up taking bath during the 4th week because the glue had all fallen off and everything seemed healed.
We had also been told in aftercare instructions that I shouldn’t wear any tight clothing, so I had been wearing very loose briefs. I found out that was wrong on day two, you need to keep the scrotum lifted against your body to prevent a hematoma, and switched back to my tighter panties. The aftercare instructions also failed to mention anything about icing the area, but that quickly became necessary. I had bought an english ice pack way back in February in preparation, and it came very much in handy. Ice not only helped to reduce the swelling and the pain, it also reduced the fluid buildup in the scrotum.
 𝓙𝓸𝓬𝓮𝓵𝔂𝓷
𝓙𝓸𝓬𝓮𝓵𝔂𝓷 
 ⚢
⚢ @TwippingVanilla
@TwippingVanilla 
 ⚢
⚢ @TwippingVanilla
@TwippingVanilla 
 ⚢
⚢ @TwippingVanilla
@TwippingVanilla Hahahaha, omg, is this what people mean when they talk about the lifting of the brain fog?
I feel more lucid right now than I have in a decade.
Fuck me, this is something else.
Hahahaha, omg, is this what people mean when they talk about the lifting of the brain fog?
I feel more lucid right now than I have in a decade.
Fuck me, this is something else.
I’m being told this may have actually been from coming off the opiates. ¯\_(ツ)_/¯
The doctor had prescribed me an opiate pain killer and a stool softener to counter the constipation from the opiate. Kat ran into problems getting the hospital pharmacy to fill the prescriptions, first because they had the wrong name on file, and then because she misremembered my birthday. The morning after the surgery she had me take both meds, but this was the last day I did. I just didn’t need them, I was completely used to pain down there, and it was already diminishing. The next few days I got by with just tylenol and ibuprofen. I was very thankful for that, because that first bowel movement on day 2 was like giving birth.
By the fourth day I was up and walking around fine, but still not allowed to drive anywhere because I kept having lightheaded spells. I wasn’t exactly dizzy, but I wasn’t stable either. Eventually we realized this was because I was so dehydrated. Coming off of Spiro, combined with the shock of the surgery, had sent my body into rapid flush mode, and I was peeing out all my moisture. It took over a week before every glass of water I drank didn’t get peed right back out shortly after. It wasn’t until the second week that I stopped having that lightheaded feeling. I also had some compounded issues from my Concerta (ADHD medication), which may have been making the lightheadedness worse. I had to stop taking it eventually.
 𝓙𝓸𝓬𝓮𝓵𝔂𝓷
𝓙𝓸𝓬𝓮𝓵𝔂𝓷 
 ⚢
⚢ @TwippingVanilla
@TwippingVanilla Wife: "Be sure to get up and move around more, don't spend all day sitting at your desk. I imagine that chair can't be good for your testicles."
Me: "Uhm... hon..."
Wife: "YOU KNOW WHAT I MEAN."
Most of the sutures had dissolved by the second week, and all but a little of the glue had fallen off. In my follow up appointment the doctor told me that I would probably have to tug on the ends of the stitches to remove them, but they should come freely (I never actually needed to, they fell out at some point). The worst of the swelling had faded by the second week, but the “grapes” remain (and still do as I write this approaching 5 weeks). Scar tissue is present along the incision, and touch sensation there feels a little weird, but it’s not all that different from the natural skin texture there, just thicker. There were also numb zones all around my scrotal tissue where I had no sensation at all. Periodically over the first two weeks I would suddenly get a sharp stabbing pain as nerves in the area reconnected. Sensation has now fully returned and all is well.
Life after T
 𝓙𝓸𝓬𝓮𝓵𝔂𝓷
𝓙𝓸𝓬𝓮𝓵𝔂𝓷 
 ⚢
⚢ @TwippingVanilla
@TwippingVanilla My skin feels softer… my gut reaction to that is placebo effect, except that the cracks on my fingers and hand are gone.
Cracks that have been there for 9 years. I got them from working at an HP server reseller. The dust destroyed my skin.
They’re gone.
The above tweet was on day 2. It wasn’t placebo, my skin really had suddenly gotten a whole lot softer. Sensation had increased too, textures became more pronounced. I remember touching my wife’s leg that evening and it felt buttery smooth in a way I’d never felt before. This was the first aspect of being completely, truly free of testosterone. Even tho my blood results showed that my T had been suppressed very well (last read pre-surgery was 10.5 ng/dL), it is pretty clear to me now that the numbers Spironolactone produces were not an accurate measure of the androgens in my body.
 𝓙𝓸𝓬𝓮𝓵𝔂𝓷
𝓙𝓸𝓬𝓮𝓵𝔂𝓷 
 ⚢
⚢ @TwippingVanilla
@TwippingVanilla *removes all the spiro from her pill planner*
Never again. God what an awful drug.
Spiro is a really garbage drug to use as an anti-androgen. Not only because it’s a diuretic, but because it causes massive spikes in cortisol levels. This prevents fat from burning properly, can cause depression, and even impairs cognitive thinking. It took three weeks for my system to get used to being off the spiro, and during those three weeks my body did not know which way was up.
One evening as I laid in the recliner in our livingroom I suddenly felt my entire body go rigid and tense up. The sensation was not all that dissimilar to the feeling I get as I build up to an orgasm; my arms and legs started twitching very very slightly. This lasted for a good 5 or 10 minutes, and when it passed I suddenly felt full of energy. It is my belief that this was my body crossing a threshold on withdrawal from either the testosterone or the spiro. Unfortunately, since both were dropped at the same time, it’s impossible for me to say.
 July 13th, 2018. San Diego Trans Pride It was after the second week that I started noticing fat changes. My waist started slimming out, as belly fat migrated away from my underbust, which itself dropped 2 inches in a week, taking me from a 44DD to a 42DDD. My belly got softer and started to change shape some, expanding out more to the sides and less in front. At San Diego Trans Pride, two and a half weeks post-op, my wife took a photo of me from behind as we walked across the park, and in it you can clearly see how I was suddenly developing a much more feminine waist.
July 13th, 2018. San Diego Trans Pride It was after the second week that I started noticing fat changes. My waist started slimming out, as belly fat migrated away from my underbust, which itself dropped 2 inches in a week, taking me from a 44DD to a 42DDD. My belly got softer and started to change shape some, expanding out more to the sides and less in front. At San Diego Trans Pride, two and a half weeks post-op, my wife took a photo of me from behind as we walked across the park, and in it you can clearly see how I was suddenly developing a much more feminine waist.
Fat migration has continued; back fat has been decreasing steadily, and the side fat along my bust is rapidly creeping away, giving me a nice flat area under my arms and providing much more shape to my breasts. I expect within the next few weeks I’ll lose another band size and will be forced to buy new bras. The reduction around my waist has also had the benefit of making my busy much more proportional and I no longer feel such a strong desire for them to be larger.
The most pleasant development to have come in the month since my surgery has been sexual function and a massive drop in dysphoria surrounding my genitals. I mentioned at the start of this article that at the beginning of my transition I felt no dysphoria surrounding my penis. That changed over the last year as penile atrophy set in and aggravated my peyronies disease. This caused erections to become not only uncomfortable, but downright painful. Combine this with the softening of genital tissues, and PiV sex became even more undesirable than it had been before. I had long abandoned masturbating like a man, having found that HRT made use of vibrators significantly more effective, and frequently I found myself more and more frustrated by erections during sexual play when I just wanted to treat my parts like a vulva and clitoris.
As nerves in my scrotum began to reconnect, I started getting sensations that I couldn’t explain. In short, my scrotum stopped feeling like a scrotum. When I would be laying or sitting still I would get sensations that felt much deeper inside my groin than I should be able to get. In short, I started experiencing a phantom vagina. My theory is that as nerve reconnected, my brain looked at it’s internal map of where each one went, saw my body was in estrogen mode, and said “Oh, this must be my vagina.” It’s a pleasant experience, but also somewhat distracting when it hits you while driving. I also noticed that certain thoughts and feelings would trigger a muscular sensation deep inside my pelvis that I had never experienced before, which I think is a new form of arousal.
The real surprise, however, came nearing the end of the fourth week. My wife indicated she was interesting in sex, and I felt healed enough to be up for the job. I won’t go into details, but this was the best PiV sexual encounter I have ever had in my life. Not only was my erectile pain seemingly gone, but sensation was off the charts, and as my climax built it was very clear that something huge had changed inside me. I had only once experienced “The Big O” prior to this, and it was as much a surprise this time as it was then.
Three weeks and three days after surgery I suddenly found myself feeling really good. My productivity was higher than normal, my mood had improved, I was thinking clearer… everything was coming up Jocelyn. It was like walking out from under a massive cloud system and suddenly feeling the light on my skin. The testosterone was gone, and the spiro with it; I felt alive, and it hasn’t stopped feeling that way since. Today marks 5 weeks since the surgery, and my pain is pretty much gone (sometimes the left cord gets angry if I’m too active). Getting an orchiectomy has proven to be the best step in my transition that I’ve taken since I took that first pill.
Update: Six months post-op
I cannot begin to express just how much an orchi has improved my own sense of self image and confidence with my body. This week I purchased my first swim suit bottom that does not have a skirt or any other mechanism of obscuring my crotch. After six months, my genitals have changed appearance so much that from most angles you cannot tell I still have a penis. It just looks like I’ve got an abnormally large clitoris and labia. Granted, a lot of that is because I’m fat and my FUPA obscures it all, but I don’t care, I look like I have a vagina! My wife keeps commenting on how feminine my genitals look, she’s thrilled by it. I’m no longer scared somebody might peek through a gap in a bathroom stall and see a protuberance.
I still significantly want GRS some day, but my genital dysphoria has shifted to being more centered on just wanting the correct parts for my fulfillment, not because it could give me away as trans. Weight migration has continued to occur; I’m now a 42F/G cup and am really close to a 40 band, my curves have fleshed out a LOT, and there is no longer anything about my shape that appears male. With that change has come a HUGE surge in body confidence, I’m finally happy in my skin.

